SERGIO AUGUSTO CAMPOLINA DE AZEREDO, M.D., MARIA MASCARENHAS, RODRIGO DE PAULA MASCARENHAS VAZ, M.D., CAMILA COHEN KALEKA, M.D., PH.D., E PEDRO DEBIEUX, M.D., PH.D.
Abstract
The integration of extra-articular procedures in anterior cruciate ligament (ACL) reconstruction is crucial, especially in the context of the high incidence of ACL injuries, which are a leading cause of knee instability and potential progression to post-traumatic osteoarthritis. Injuries to the anterolateral ligament (ALL) and knee capsule are present in nearly 90% of ACL ruptures and are associated with significant rotational instability and grade 3 pivot-shift displacement. This study outlines a technique using the internal brace, a biocompatible device made of ultra-high-molecular-weight polyethylene fibers, not only to augment the ACL reconstruction but also to reinforce the ALL repair. Historically used across various ligament reconstructions, the internal brace aims to enhance postsurgical stability of the knee without increasing morbidity. This approach combines primary ACL reconstruction through arthroscopy with percutaneous reinforcement of the ALL. The method is designed to improve knee function and stability after reconstruction, thereby reducing the risk of ACL rerupture, protecting meniscal repairs, and increasing the rate of return to preinjury athletic performance.
Surgical Technique
Patient Preparation and Bony Landmarks
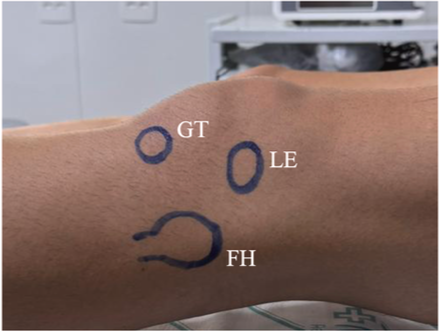
All patients provide informed consent before undergoing ACL reconstruction augmented with the internal brace, as well as ALL repair with internal brace augmentation. The patient receives standard preoperative antibiotics and is placed in the supine position under spinal anesthesia combined with an ultrasound-guided femoral nerve block. The leg is positioned with the knee free to move from full extension to 90° of flexion. An examination under anesthesia confirms ACL and anterolateral instability including grade 3 pivot shift. A tourniquet is applied around the proximal thigh, and the leg is prepared and draped in a sterile fashion. Bony landmarks are identified, including the lateral epicondyle, Gerdy tubercle, and fibular head (Fig 1). The indications and contraindications of this technique are shown in Table 1.
Indications and Contraindications of Technique
Indications
- Total tears of both ACL bundles;
- Ideal conditions for technique typically observed when surgery is performed within 14 days after injury;
- High-performance athletes;
- Anatomic factors such as intercondylar notch width or lateral condyle width are not considered limitations.
Contraindications
- Chronic or degenerative lesions associated with ACL;
- Multiligament injuries;
- Associated lesions with displaced fractures;
- Presence of open growth plate;
- ACL, anterior cruciate ligament.
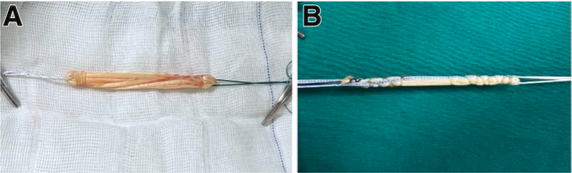
Graft Harvesting and Preparation
Femoral and Tibial Tunnel Preparation for ACL Reconstruction
An accessory anteromedial portal is established under direct visualization (Fig 3). The native ACL footprint is debrided, and an anatomic femoral tunnel is created, positioned between the lateral intercondylar ridge anteriorly and the posterior articular cartilage border of the lateral femoral condyle, using a 105° arthroscopic offset guide (Fig 3). A 2.4-mm guidewire is drilled through the lateral femoral cortex, followed by retrograde reaming using a FlipCutter (Arthrex) to the desired diameter (8-9 mm) and a depth of approximately 30 mm. A shuttle suture is left in place for later graft passage.
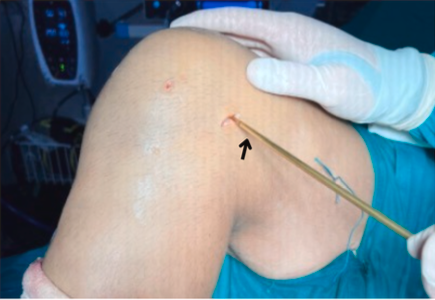
Femoral Tunnel Preparation for ALL Reinforcement
Tibial Tunnel Preparation for ALL Reinforcement
Internal Brace Reinforcement of ALL

ACL Graft Passage and Fixation
The ACL graft is pulled through the tibial tunnel into the joint and femoral tunnel using the shuttle sutures (Fig 7). Under direct arthroscopic visualization, femoral fixation is achieved using the TightRope button, which is deployed over the lateral femoral cortex. The graft is pre-tensioned at full extension with posterior drawer applied.

Tibial fixation is achieved with a bio-composite interference screw (Arthrex) with the knee in full extension (Fig 8). The FiberTape used for ACL reinforcement is tensioned intraoperatively using the “finger tension” technique. This approach optimizes the FiberTape’s role as a backup stabilizer while avoiding stress shielding.

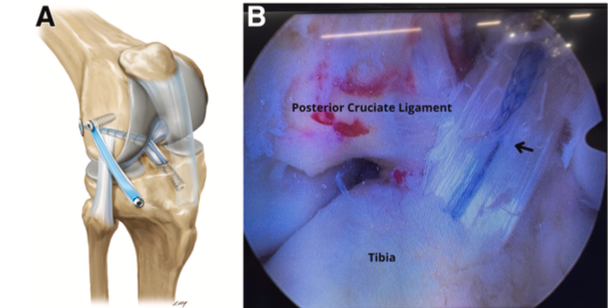
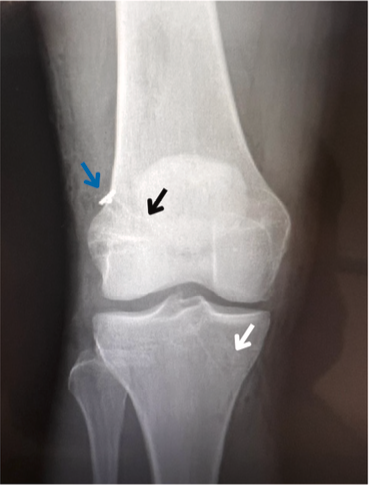
The final construct is schematically illustrated in Figure 9A, and its intra-articular placement within the knee joint is depicted in Figure 9B; the corresponding radiograph is presented in Figure 10. The whole surgical procedure is shown in Video 1. The advantages and disadvantages are shown in Table 2, and tips and pearls for the aforementioned surgical steps are shown in Table 3.
Advantages and Disadvantages
Advantages
- Anterolateral augmentation of the knee is achieved without the need to harvest the iliotibial band, preserving native tissue and reducing morbidity.
- The use of the internal brace not only allows for early mobilization but also significantly reduces the rehabilitation period. This results in a facilitated early range of motion postoperatively, enabling a quicker and safer return to high-performance sports activities. The technique optimizes recovery outcomes, which is particularly beneficial for athletes and those engaged in active lifestyles.
- Relative to other extra-articular reconstruction techniques, this method shows a decreased incidence of postoperative pain and swelling, including anterolateral discomfort and joint effusion.
- Relative to other extra-articular reconstruction techniques, this method shows a decreased incidence of postoperative pain and swelling, including anterolateral discomfort and joint effusion.
- This technique enhances rotational stability of the knee, particularly in high-risk movements associated with pivot-shift events, which significantly reduces the chances of rerupture.
The use of distinct femoral tunnel drilling techniques ensures divergent trajectories, preventing tunnel convergence at the femur.
Disadvantages
- Long-term outcomes are not yet established.
- In patients with larger anatomic structures, there is a risk of creating non-isometric tunnels.
- This technique requires precise tunnel placement and graft tensioning, demanding high surgical skill and experience. Missteps in these areas can lead to suboptimal outcomes.
- Although internal bracing is intended to enhance stability, incorrect placement or tensioning can increase stress on the graft, potentially leading to premature wear or failure.
- The addition of ALL reconstruction and the use of multiple tunnels can extend the duration of surgery.
- ALL, anterolateral ligament.
Tips and Pearls
| Surgical Step | Tips and Pearls |
|---|---|
| Tunnel planning | Ensure accurate positioning of the femoral and tibial tunnels in an isometric manner to avoid undue stress on the graft or FiberTape. |
| FiberTape tensioning | Leave the internal tape slightly loose during fixation to prevent overload on the graft, protecting against premature wear. |
| Use of anatomic guides | Use specific guides to ensure correct angulations in tunnels and avoid compromising the reconstruction. |
| Graft preparation | Ensure the graft has a minimum diameter of 8 mm and sufficient length for adequate stability within the tunnel. |
| Tunnel drilling and graft transposition | Perform femoral and tibial tunnel drilling initially, but reserve the transposition and fixation of the graft for the ACL after all extracapsular procedures (internal bracing for the ALL). |
| Supervised rehabilitation | Initiate controlled passive mobilization soon after surgery to ensure safe and effective recovery. |
ACL, anterior cruciate ligament; ALL, anterolateral ligament.
Postoperative Management
Discussion
Disclosures
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: C.C.K. reports a consulting or advisory relationship with Geistlich Pharma and Arthrex and receives speaking and lecture fees from Geistlich Pharma. P.D. reports a consulting or advisory relationship with Geistlich Pharma and Arthrex. All other authors (S.A.C.d.A., M.M., R.d.P.M.V.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary Data (1)
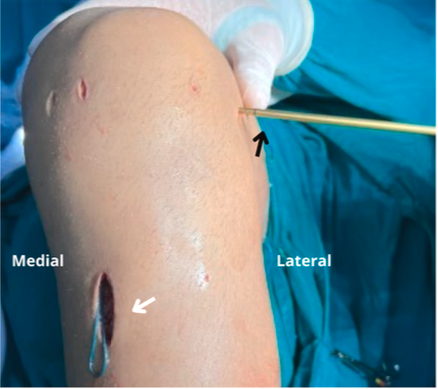
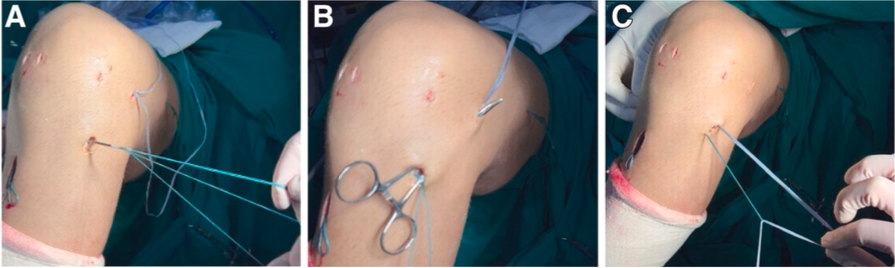
Key steps of the procedure. A percutaneous incision in the lateral knee creates access for guidewires that form the femoral and tibial tunnels. A proximal SwiveLock anchor and FiberTape secure the anterolateral ligament (ALL) reinforcement. Finally, the anterior cruciate ligament (ACL) graft is transposed and fixed with a TightRope button and a bio-composite screw, with final fixation in full extension and confirmation of knee stability.
References
1. Helito CP, Sobrado MF, Moreira da Silva AG, et al. The addition of either an anterolateral ligament reconstruction or an iliotibial band tenodesis is associated with a lower failure rate after revision anterior cruciate ligament reconstruction: A retrospective comparative trial. Arthroscopy 2023;39:308-319.
2. Helito CP, da Silva AGM. Editorial commentary: Lateral extra-articular augmentations in anterior cruciate ligament (ACL) reconstruction reduce ACL graft failure and secondary meniscectomy and are indicated for ACL primary and revision reconstruction [published online April 20, 2025]. Arthroscopy. https://doi.org/10.1016/j.arthro. 2025.04.018.
3. Hazzard S, Bacevich B, Lustig M, Lonati D, Asnis P. Preferences including graft choice, lateral augmentation, and rehabilitation after ACL reconstruction among NFL team orthopedic surgeons [published online May 8, 2025]. Arthrosc Sports Med Rehabil. https://doi.org/10.1016/j.asmr. 2025.101161.
4. Jorge PB, Toledo MB, Malpaga JMD, et al. Anterior cruciate ligament reconstruction and double extra- articular reinforcement. Arthrosc Tech 2025;14:103456.
5. Mok YR, Wong KL, Panjwani T, Chan CX, Toh SJ, Krishna L. Anterior cruciate ligament reconstruction performed within 12 months of the index injury is associated with a lower rate of medial meniscus tears. Knee Surg Sports Traumatol Arthrosc 2019;27:117-123.
6. Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am 2002;84:1560-1572.
7. Anderson AF, Snyder RB, Lipscomb AB. Anterior cruciate ligament reconstruction. Am J Sports Med 2001;29:272-279.
8. Ferretti A, Monaco E, Gaj E, et al. Risk factors for grade 3 pivot shift in knees with acute anterior cruciate ligament injuries: A comprehensive evaluation of the importance of osseous and soft tissue parameters from the SANTI Study Group. Am J Sports Med 2020;48:2408-2417.
9. Monaco E, Helito CP, Redler A, et al. Correlation between magnetic resonance imaging and surgical exploration of the anterolateral structures of the acute anterior cruciate ligament—injured knee. Am J Sports Med 2019;47: 1186-1193.
10. Helito CP, Helito PVP, Costa HP, Demange MK, Bordalo-Rodrigues M. Assessment of the anterolateral ligament of the knee by magnetic resonance imaging in acute injuries of the anterior cruciate ligament. Arthroscopy 2017;33: 140-146.
11. Bernholt DL, Kennedy MI, Crawford MD, DePhillipo NN, LaPrade RF. Combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis. Arthrosc Tech 2019;8:e855-e859.
12. Helito CP, Bonadio MB, Gobbi RG, et al. Combined intra-and extra-articular reconstruction of the anterior cruciate ligament: The reconstruction of the knee anterolateral ligament. Arthrosc Tech 2015;4:e239-e244.
13. Dadoo S, Herman ZJ, Hughes JD. Surgical techniques in primary ACL reconstruction. Clin Sports Med 2024;43: 399-412.
14. Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BHB, Murphy CG, Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-Year follow-up. Am J Sports Med 2015;43:1598-1605.
15. van der List JP. Editorial commentary: Proper graft choice and lateral extra-articular tenodesis are key to successful anterior cruciate ligament reconstruction in female soccer players [published online April 24, 2025]. Arthroscopy. https://doi.org/10.1016/j.arthro.2025.04.029.
16. Granan LP, Bahr R, Lie SA, Engebretsen L. Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears. Am J Sports Med 2009;37:955-961.
17. Inderhaug E, Stephen JM, Williams A, Amis AA. Anterolateral tenodesis or anterolateral ligament complex reconstruction: Effect of flexion angle at graft fixation when combined with ACL reconstruction. Am J Sports Med 2017;45:3089-3097.
18. Tashman S, Collon D, Anderson K, Kolowich P, Anderst W. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med 2004;32:975-983.
19. Park YB, Lee HJ, Ro DH, Lee GY, Kim S, Kim SH. Anterolateral ligament injury has a synergic impact on the anterolateral rotatory laxity in acute anterior cruciate ligament-injured knees. Knee Surg Sports Traumatol Arthrosc 2019;27:3334-3344.


